Acupuncture and Coccydynia
One of the most specialized applications of Acupuncture concerns coccygodynia (correct) or coccydynia (shortened) either as the result of trauma or as treatment (rather than cure) of chronic regional pain of unknown etiology. As repeatedly mentioned, Acupuncture is now regarded Complementary Medicine rather than alternative therapy and its use is particularly indicated, whenever a therapeutic vacuum is found, i.e. when Western Medicine offers no viable option. Unfortunately for Western Medicine, coccydynia is nothing but a huge therapeutic vacuum.
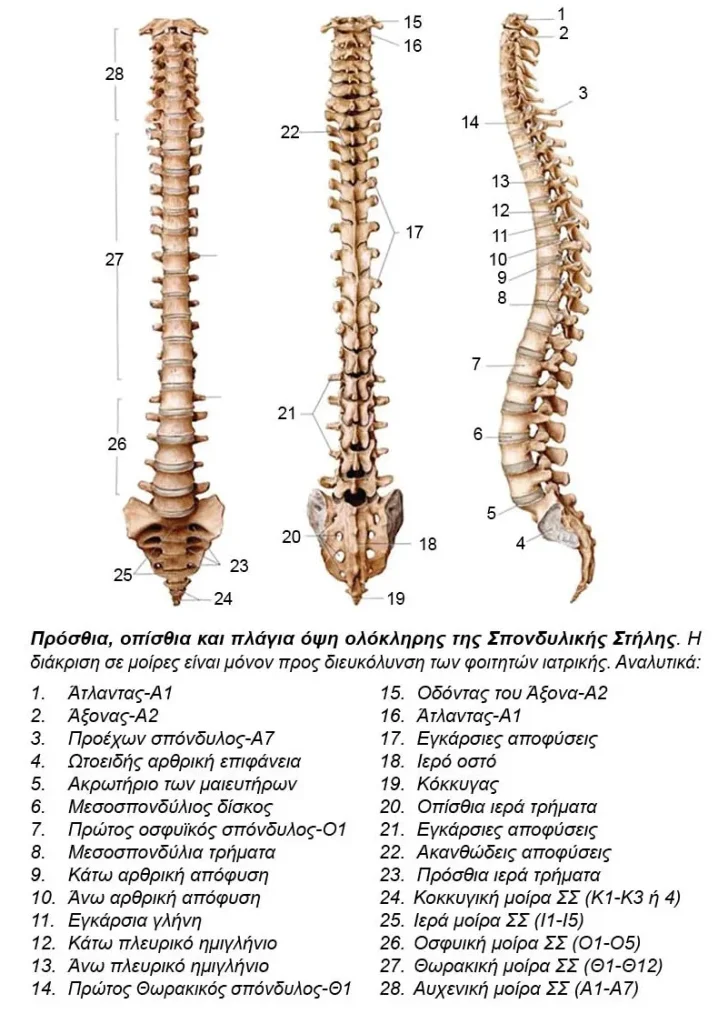
The spine is usually classified into Cervical, Thoracic, Lumbar, Sacral and Coccygeal parts, with the last two usually examined together. The reason is simple. Both the sacrum and the coccyx are ossified, they are not (fully) separated by intervertebral discs and form respectively the sacrum and the coccyx. The sacrum is considered the cornerstone of the pelvic ring and ensures the smooth transition of loads and body weight from the trunk to the pelvis and from there on to the lower extremities. The coccyx is considered a “residual” bone, since in other animals, including several Primates, it forms the beginning of the tail, while in Homo Erectus and much later in Homo Sapiens Sapiens it does not seem to have an “apparent” function. This is not equivalent to saying that it has no function at all, as it may very well have unknown properties and functions.
Eastern medicine and Martial Arts believe that a strike to the coccyx region or pelvic floor may prove fatal. However, Western medicine provides no scientific explanation for backing up such claims. Nevertheless, two residual structures in the coccyx area should be referenced. The first concerns the “azygo nerve ganglion” or Walther’s ganglion or ganglion impar, a nerve formation with fibers of the autonomic nervous system. The second structure is supplied by the terminal branch of the middle sacral artery and resembles the carotid bulb, a neural or rather neurogenic formation within a vascular structure, so possible names include “coccygeal bulb” or body or gland or ganglion of Luschka, named after the German anatomist Hubert Luschka (1820–1875).
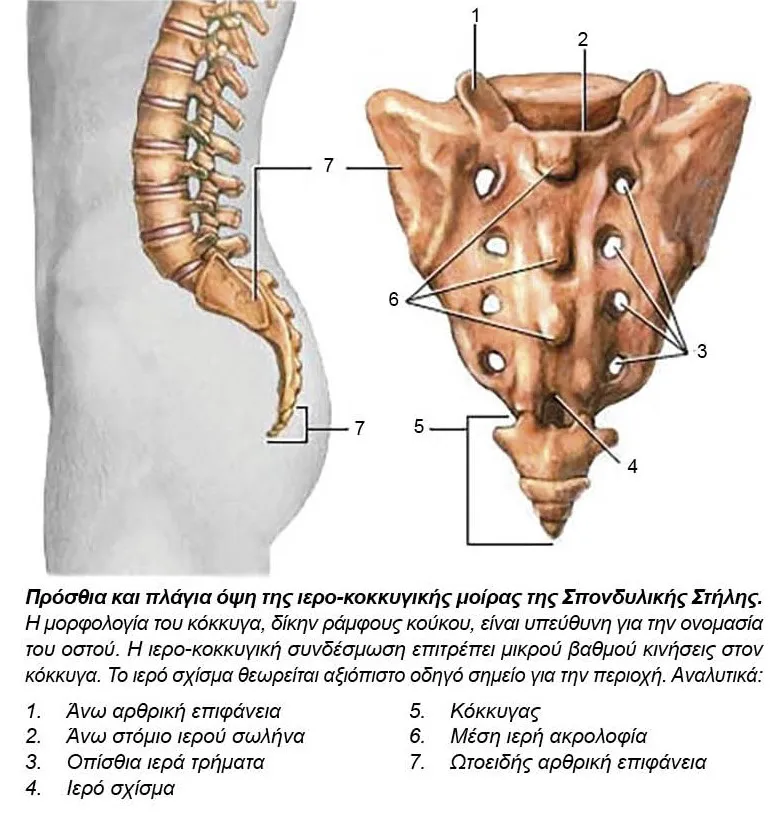
In medicine, as indeed in life, we very often realize the importance of an organ either through its aplasia or after its iatrogenic removal or traumatic loss or when we eventually realize that what we do know is probably much less than what we do not know. One of the topics we definitely ignore is the function of the coccyx, to which, despite its hypoplasia, very strong muscles and ligaments of the pelvic floor are still attached.
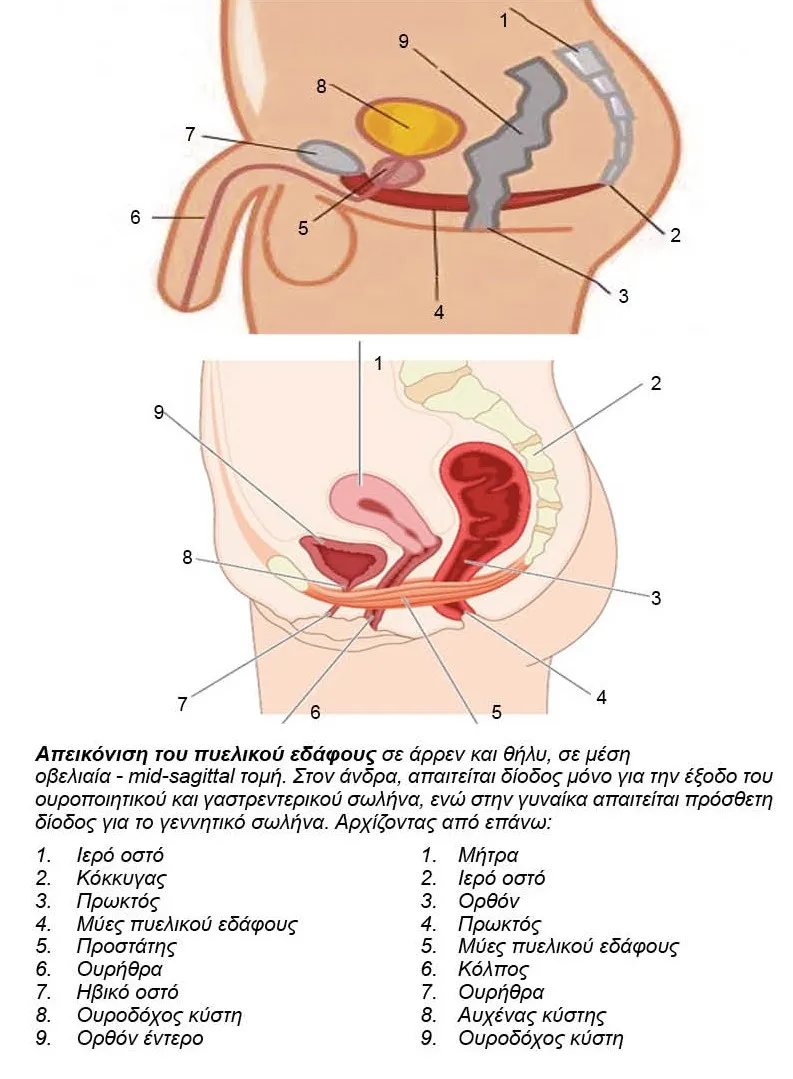
The pelvic floor is different in men and women, not so much because the muscles and other anatomical elements are different, but because its function is different. Even its openings – weak spots of the pelvic floor are different.
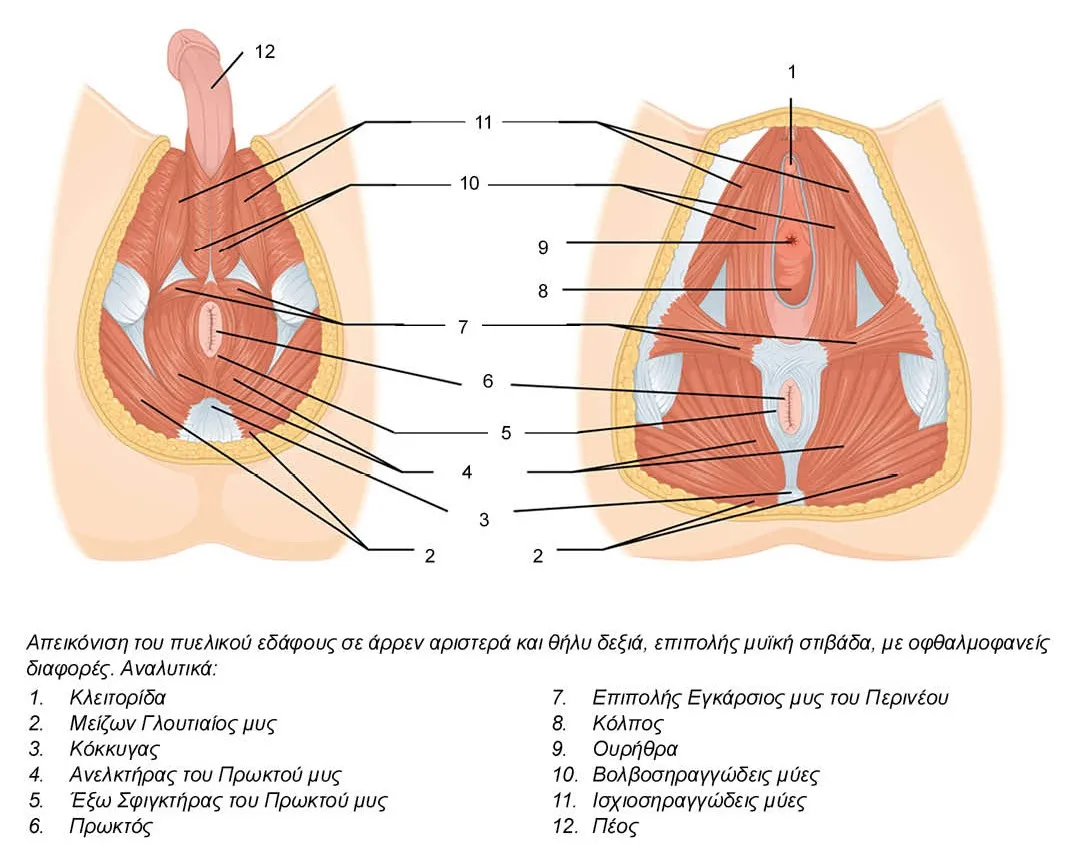
In the male body, one passage is required for the exit of the urinary and another one for the gastrointestinal tract for a total of two openings – weak spots. On the other hand, in the female body, an additional passage is required, and gets especially stressed out, when called upon to perform its role in reproduction.
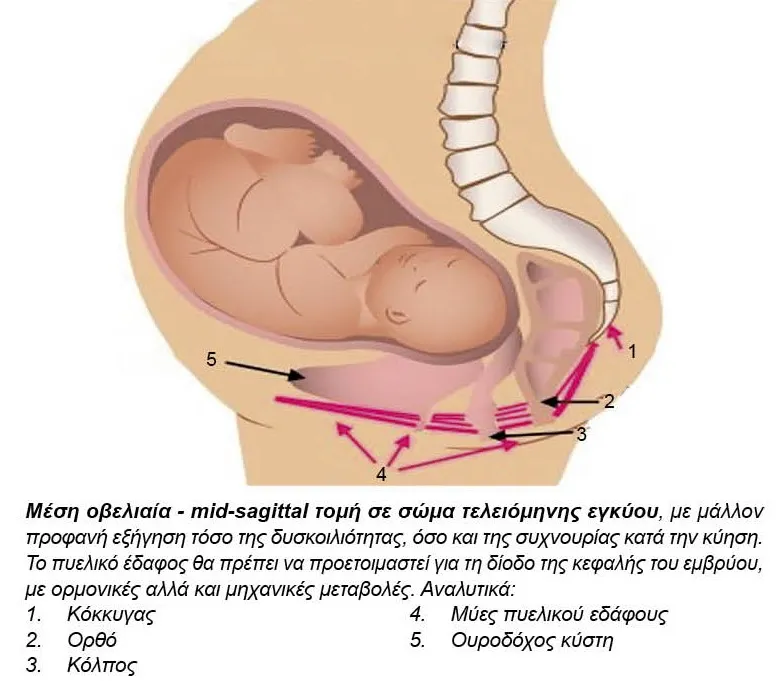
Thus, the entrance of the vagina, turns during childbirth into an exit for the fetus and it expands terribly in conjunction with the loosening of the symphysis pubis. If osteoarthritis of the pubic symphysis is to be expected in multiparous women, why is it not equally plausible that similar lesions have occurred in both the vagina and the coccyx? Therefore, coccydynia should not be surprising in multiparous women.
On the contrary, the occurrence of coccydynia in women who have not experienced labour is particularly troubling, especially when it is accompanied by mental disorders, extremely common in any chronic pain and much more so in this specific anatomical location, which makes it unimaginably difficult to report in the first place and to seek the appropriate medical care thereafter.
It makes sense that when Western Medicine identifies the cause and offers an effective treatment, then most physicians would opt for Western Medicine. However, when Western Medicine either does not know the cause of the so-called idiopathic diseases, or when it knows the cause, but no effective treatment is available, then it makes perfect sense to seek the assistance of Complementary and Alternative Medicine, with a self-evident preference for the methods that have stood the test of time. Second postulate, equally self-evident as the first, is the inadequacy of the pharmaceutical approach. The administration of painkillers and anti-inflammatory drugs has a place in the treatment of pain. However, chronic administration of painkillers and anti-inflammatory drugs has no place in the treatment of chronic pain. Other, non-pharmaceutical, solutions are therefore sought for a theoretically simple problem. Such solutions could be special pads with a gap in the painful area, inflatable rings similar to the ones used in hemorrhoids, wearable pads-shorts, with reinforcement and protection in the coccyx area, similar to the Hip protectors, which have reinforcement and protection in the trochanter area, taping in the disputed area or special straps, similar to those used in epicondylitis of the elbow or osteochondritis of the tibial tuberosity.

In terms of clinical examination and differential diagnosis, we should be able to distinguish between the anatomical variant, known as Hooked coccyx, with acute angulation between the adjacent coccygeal vertebrae, which apparently does not require treatment, from the fracture – dislocation of the coccyx, which presupposes history of trauma and probably requires treatment. The pain presentation usually (but not always) provides the solution, while the clinical examination itself being difficult, unpleasant or psychologically charged. In fact, for purely legal reasons, it should always be preceded by detailed information of the patient and written informed consent.
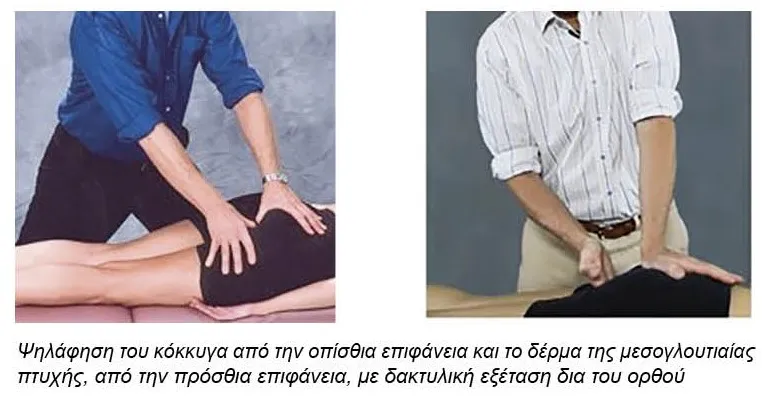
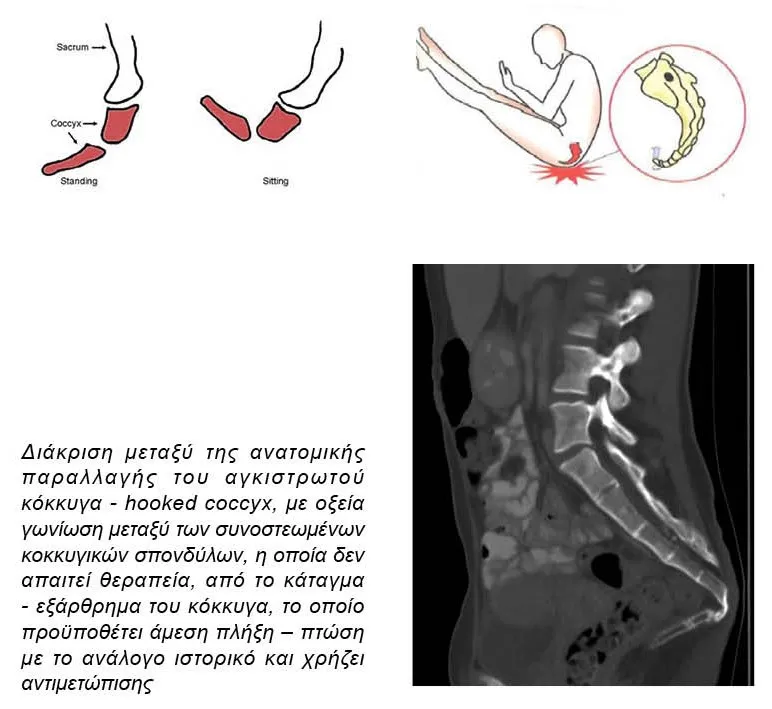
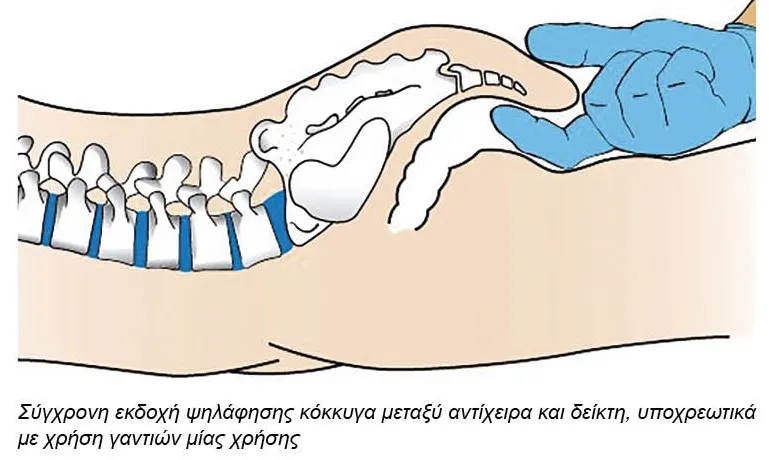
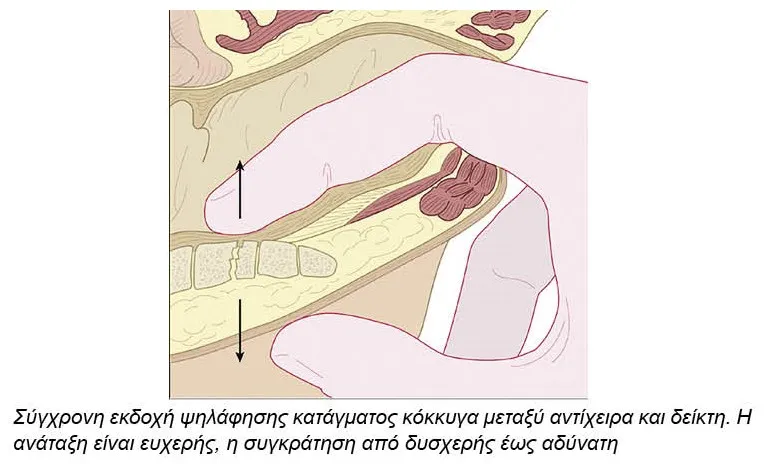
Palpation of the coccyx is done by grasping the bone between the rectum and the overlying skin and, totally theoretically, reduction of a fractured coccyx may be achieved with the same mechanism. Whether this is possible without general anesthesia is highly debatable. Even if a reduction may be achieved, it is equally debatable whether it may be retained.

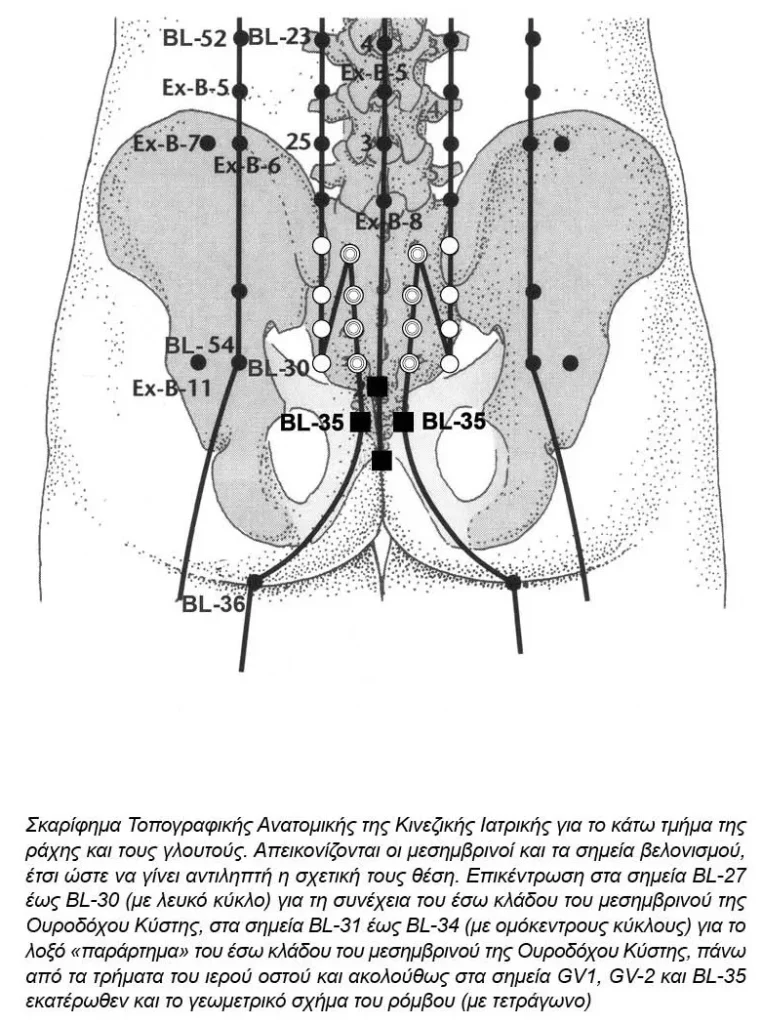
Consequently, a therapeutic vacuum is definitely identified in the treatment of Coccydynia and in this case, Acupuncture, in the absence of any other effective therapeutic intervention, can be of crucial importance. Pain management can be started as initial and non-specific, as with the Opening the four gates – Siguan approach (LI-4 & LIV-3 bilaterally), with only 4 needles, feasible even in the Emergency Department. Attention is required regarding the excessive manipulation of the acupuncture point LI-4, in the first interdigital space, as iatrogenic damage in the area has been reported. Treatment may be continued based on the established criteria for selecting acupuncture points, as they apply for other areas of the body. It may be wise to view Coccydynia as Extremely-Low-Non-Specific-Back-Pain, the only difference being that the acupoints converge too much towards the midline and eventually become practically inaccessible. Therefore, point selection starts with the sensitive – painful – Ashi points, first choice for both physician and non-physician acupuncturists. The latter are also referred to as Licensed Acupuncturists – Lic. Ac, requiring a specific study curriculum and usually strict exams, set by a governing body. In Greece, they are officially absent, as there is no corresponding official curriculum nor governing body. The problem is usually solved the Greek way “you are what you claim to be“.
Regarding the selection of acupuncture points, next rational choice is the Huatuo Jiaji points – EX-B-2, which practically prove the early recognition of Neuro-Anatomical Acupuncture by Chinese Medicine, again a common choice for both physician and non-physician acupuncturists. Most medical acupuncturists admit that the theory of Zang-Fu Organs has little influence on their choice of acupuncture points. In fact, the interaction of Western and Eastern Medicine has begun to adversely influence the selection of points with Chinese physicians accepting the Western minded rationale.
Acupoints suitable for use in Coccydynia are as follows: GV-1, as a local point, but also as a Luo-connecting point of the GV meridian, SI-3, as a control point – master point of meridian GV, BL-31 to BL-34, bilaterally, as a set of local points for the region of the sacrum and coccyx, BL-35 as a local point for haemorrhoids, prolapse of the rectum and diseases of the coccyx, BL- 57 and/or BL-58, as remote points for the region of the sacrum and coccyx, with an official indication of hemorrhoids and diseases of the rectum.